Shockwave Treatment of Erectile Dysfunction
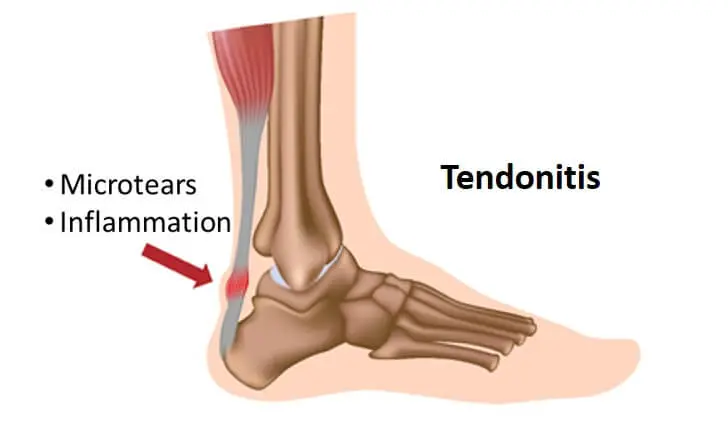
Low-intensity extracorporeal shock wave therapy (LI-ESWT) is a novel modality that has recently been developed for treating erectile dysfunction (ED). Unlike other current treatment options for ED, all of which are palliative in nature, LI-ESWT is unique in that it aims to restore the erectile mechanism in order to enable natural or spontaneous erections. Results from basic science experiments have provided evidence that LI-ESWT induces cellular microtrauma, which in turn stimulates the release of angiogenic factors and the subsequent neovascularization of the treated tissue. Extracorporeal shock wave therapy (ESWT) has been clinically investigated and applied in several medical fields with various degrees of success.