Signs Your Plantar Fasciitis is Healing
Vessel Crew
on
June 1, 2023
Signs Your Plantar Fasciitis is Healing

By Vessel Crew
Intro
If you have plantar fasciitis, you know the pain that can come with every step and how it can negatively affect your life. It is almost impossible to avoid using your feet, and the recovery process can be long and frustrating.
Luckily, your plantar fasciitis will heal, and you will eventually take a pain-free step. You may not realize the progress at first, but slowly you will have fewer plantar fasciitis symptoms. Is your plantar fasciitis healed? Is it ok to start jumping back into activities that you had previously stopped? Can you start wearing less supportive footwear? Starting activities too early and wearing unsupportive footwear can be risky and set back your recovery if your plantar fasciitis has not fully healed. It is essential to know the signs of a healthy plantar fascia and signs that you need a little bit more time and rest.
Below are some key signs your plantar fasciitis is healing and some tips to help you in the recovery process.
What is Plantar Fasciitis?
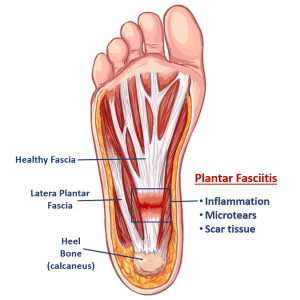
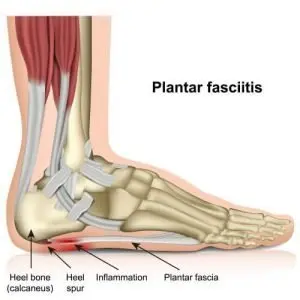
First, what is plantar fasciitis? Plantar fasciitis is a widespread cause of heel pain that affects about 10% of the U.S. adult population. The plantar fascia is a long flat ligament on the bottom of your foot. It connects your heel bone to your toes to support the arch of your foot. Like other ligaments in your body, it can stretch within limits and then return to normal.
If too much tension and stress are applied, small tears can form in the fascia, and it becomes inflamed. Unfortunately, we rarely give the fascia enough time to properly heal, so the body patches the inflamed fascia with scar tissue.
Repeatedly doing this over months or years causes more tears and scar tissue until your fascia is in a state of degeneration with chronic pain. Those small scar tissue areas have formed a large area of scar tissue, a disorganized mess of collagen, nerves, and blood vessels. This disorganized tissue inhibits your body from healing the injury and causes chronic pain.
Symptoms of plantar fasciitis can include:
- Sharp, stabbing pain in your heel
- Radiating pain in the heel and ankle
- Reduced range of motion in foot and ankle
- Bruising or swelling on the bottom of your foot
- Difficulty walking, standing, or running
- Dull aching pain or cramp through your arch or from your heel to your toes
We will discuss common treatment options later, but first, let us talk about a few signs your plantar fasciitis is healing.
Signs your Plantar Fasciitis is healing
Knowing the indicators of plantar fasciitis healing are important for recovery. Some of the key signs that your plantar fasciitis is healing are listed below.
1. Your First Steps in the Mornings Are Easier
One of the most prominent signs of plantar fasciitis is a sharp, stabbing pain you may feel with your first steps in the morning. A lack of pain when you get out of bed is one of the first signs that your plantar fasciitis is healing. Why does it feel better? A lack of pain in the morning indicates a reduction in inflammation.
Be careful to keep up the therapeutic activities that got you to this point. For example, keep wearing your supportive shoes or orthotics that help provide cushioning and support to the fascia.

2. Your Pain is Becoming More Localized
Plantar fasciitis pain can radiate from your foot and heel into the ankle and calf. This pain can affect how you walk, leading to pain in your knees, hips, and lower back.
If you notice a reduction in pain in these areas, this is a good sign that your plantar fasciitis is healing. With a reduction in pain, you have probably started walking more normal, thereby reducing stress on your knees, hips, and back. You may still have localized pain in your foot, but reducing the radiating pain is a good step forward.

3. Your Range of Motion is Improving
Stretching is an often overlooked but necessary plantar fasciitis treatment. Stretching can be painful because the fascia is inflamed, but stretching can help strengthen and elongate the fibers to handle stress better.
If you notice that your foot and calf stretches are becoming easier, this is a sign that your range of motion is improving and that healing has begun. Your ability to move your toes and foot through a broader range of motion is a good sign your plantar fasciitis is healing.

4. Swelling and Bruising are Fading
If you suffer from severe plantar fasciitis, you may have noticed swelling or bruising around your arch or heel. These symptoms indicate that your plantar fascia is inflamed and most likely has microtears. Not everyone experiences these symptoms, but do not get frustrated if you have. If you noticed your foot is less swollen or bruised, that is a good sign that you are on the way to recovery.
Healing plantar fasciitis takes time and rest. It is a relief when your foot is starting to feel better, and you see signs of healing, but be careful to keep up the stretches and therapies that get you to this point. While the facia heals, patience can be difficult, but it is necessary as healing requires time and rest. How long does it take to heal plantar fasciitis?

How Long Does Plantar Fasciitis Last?
Plantar fasciitis is most often a result of years of stress that damage the plantar fascia. Healing plantar fasciitis can take a long-time, often because it is challenging to stay off your feet and give them the rest necessary for healing. There is a range for recovery times, but for those that catch it early and follow self-care or doctor-directed treatments, the average time is six months.

A pound of prevention is worth an ounce of cure, even for plantar fasciitis. Understanding what causes plantar fasciitis may help you prevent this painful condition. To learn how to prevent plantar fasciitis, you can read our blog here. While six months seems like a long time, ignoring plantar fasciitis may make a recovery a lot longer. The following are some common plantar fasciitis treatments.

How Long Does Plantar Fasciitis Last?
For most people suffering from plantar fasciitis, recovery is about 6-months with conservative treatments. These plantar fasciits treatments range from therapies you can do at home, such as icing and rest, to treatments your doctor may recommend, such as physical therapy.
Most people start with icing, rest, and nonsteroidal anti-inflammatory drugs (NSAIDs) to decrease inflammation and reduce pain.
Utilizing supportive footwear and orthotic inserts is an excellent way to decrease your foot’s stress by providing cushioning and support.
A doctor may also recommend physical therapy or night splints to stretch and strengthen your fascia. A steroid injection may also be considered to reduce inflammation and relieve pain. Be careful, though; multiple injections may weaken the fascia and cause additional damage.
If you have done all these conservative treatments but still have plantar fasciitis pain, your doctor may recommend plantar fasciotomy surgery or non-invasive High-energy Extracorporeal Shockwave Therapy treatment.
OrthoWave® is an FDA-approved, High-energy Extracorporeal Shockwave Therapy (HeSWT) treatment that is a non-invasive alternative to surgery. Only a single session of OrthoWave® is needed, and there is no downtime after your treatment, unlike surgery. Since 2010, HeSWT is recommended over the surgery by the College of Foot and Ankle Surgeons because it is exceptionally safe and highly effective.

Conclusion
Plantar fasciitis is painful, and the road to recovery looks a little bit different for each person. There are a few common signs your plantar fasciitis is healing and knowing these are important. If you do not see signs of healing, you do not have to live with the pain of plantar fasciitis. There are numerous treatment options when others have failed, including surgery or Orthowave HeSWT. The important thing is that you get you back on your feet and doing the things you love again, pain-free.
Latest Posts
Based In Science, Elevated by Service
Based In Science, Elevated by Service By Vessel Crew Vessel’s passion for improving the lives of others is anchored in an enthusiasm for science and its basis in wellness. Since our founding,…
NADH, NAD+, And NAD Benefits, Side Effects, Dosage And Stacking
NADH, NAD+, And NAD Benefits, Side Effects, Dosage And Stacking By Vessel Crew Let’s learn a little about this co-enzyme called NAD. It can be referred to as NADH, NAD+, NAD, vitamin…